- Solutions
-
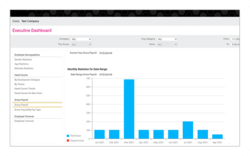
- Payroll
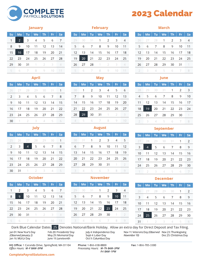
Payroll tax filing, automated and integrated processing, paperless reporting and more.
- Talent Management
Personalized recruiting, onboarding, performance management, training and offboarding.
- HR Solutions
HR support, handbook development, training, safety and compliance — all the daily tasks of people management.
- Payroll
-
- Benefits
Comprehensive and affordable medical, dental, retirement, workman’s comp and pre-tax savings plans.
- Time & Attendance
Integrated time and attendance tracking, PTO request and accrual management, scheduling and reporting.
- Employee Engagement
Custom experiences designed to attract, engage, and retain talent to get the best from your staff.
- Benefits
-
- Who We Serve
-
- Startups
Start strong with personal service that will grow with you as you scale your business.
- Small & Medium Businesses
Grow and evolve with strategic guidance and all-in-one solutions for payroll, HR and benefits.
- Large & Enterprise Businesses
Discover custom systems and integrations with industry-leading technology to help reduce administrative burden and increase your bottom line.
- Startups
-
- Resources
- Who We Are